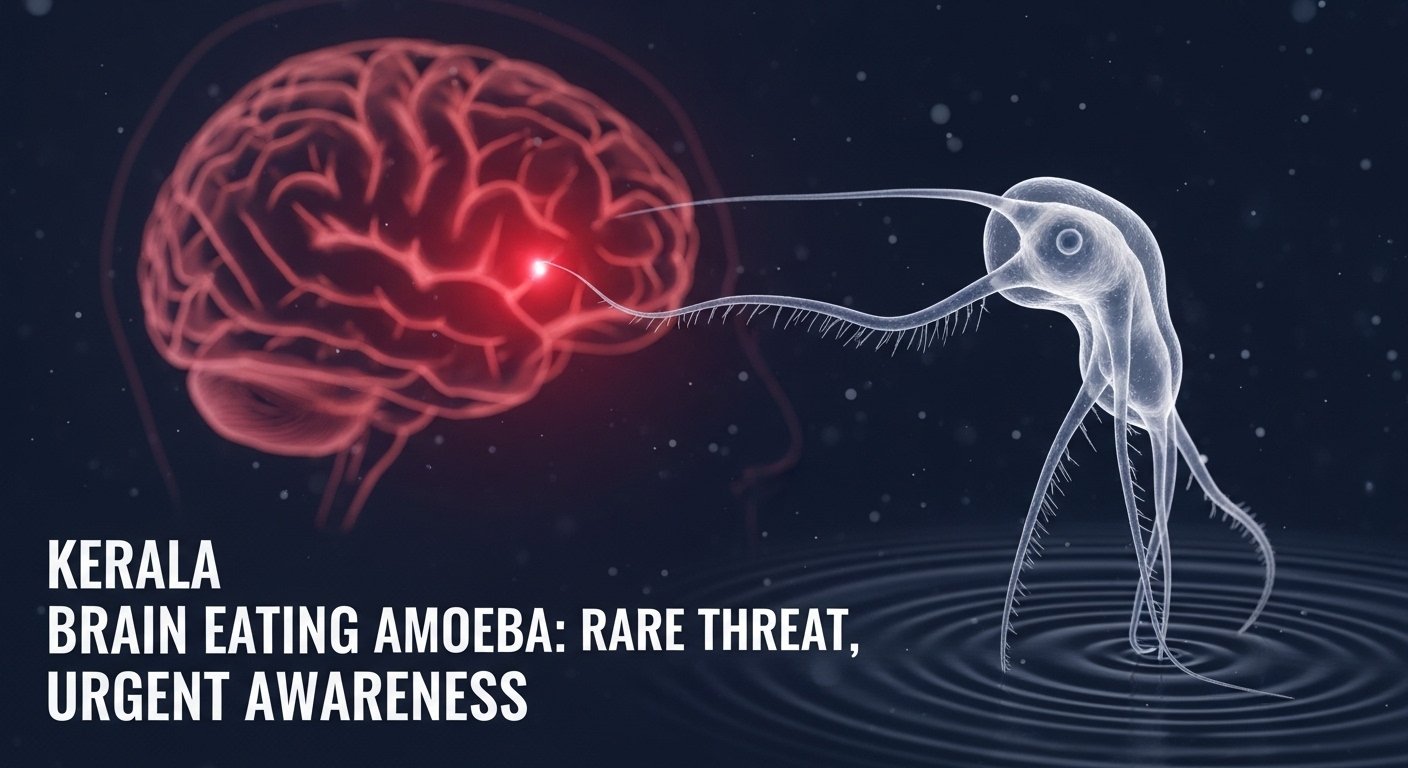
In recent months, the term Kerala brain eating amoeba has emerged in headlines across India and beyond. What once seemed a remote menace has now surged into public awareness. The deadly infection tied to the amoeba known as Naegleria fowleri, also called the “brain-eating amoeba”, has prompted alarm in the southern Indian state of Kerala. Reports show that warm, poorly chlorinated freshwater bodies and other risk factors are fueling cases of the rare yet almost invariably fatal disease known as primary amoebic meningoencephalitis (PAM). In this article, we’ll unpack what Kerala brain eating amoeba means, how it spreads, what signs to look out for, what’s being done in response — and most importantly, how individuals and communities can protect themselves.
What is the Kerala Brain Eating Amoeba?
When you encounter the phrase Kerala brain eating amoeba, it refers specifically to cases of infection by Naegleria fowleri in Kerala. This free-living protozoan thrives in warm freshwater, enters the human body via the nasal passages, travels along the olfactory nerve, reaches the brain and causes a swift, destructive inflammation of brain tissue. Globally, it’s exceedingly rare but carries an extraordinarily high fatality rate—often over 95%.
You Might Also Like: Pintola High Protein Oats
In Kerala specifically, the state health department has reported dozens of cases in recent years, making the term “Kerala brain eating amoeba” a shorthand for this public-health concern.
Why is Kerala Experiencing This Surge?
Several key factors come together in Kerala’s climate and infrastructure that elevate the risk of the Kerala brain eating amoeba phenomenon:
- The tropical environment, warm temperatures, and abundant freshwater bodies create ideal breeding grounds for the amoeba.
- Stagnant or shallow water in ponds, rivers, wells and poorly maintained swimming pools offers favourable conditions for the amoeba to proliferate.
- Traditional water-use practices — such as bathing in natural bodies of water, nasal irrigation (jala neti) with untreated water — may increase exposure risk.
- Gaps in water sanitation, leftovers of older infrastructure, low chlorination, and lack of awareness add to the threat.
- Environmental changes, including climate variations and erratic rainfall, may be amplifying risk in these warm water habitats.
Because of this confluence of factors, Kerala has become a hotspot for tracking the Kerala brain eating amoeba issue — prompting authorities to respond.
How the Infection Occurs
Understanding the mechanism of infection sheds light on how the Kerala brain eating amoeba enters and progresses:
- The amoeba resides in warm freshwater or inadequately sanitized water bodies.
- An individual enters or swims in this water — especially activities where water may enter the nose (diving, submerging head, nasal rinsing).
- Water containing Naegleria fowleri travels up the nasal passages, crosses the cribriform plate via the olfactory nerves, and reaches the brain.
- Once in the brain, the amoeba causes rapid inflammation, brain-tissue destruction, hemorrhage, and swelling — typically leading to death within days.
- The infection is not spread from person to person; rather, it is a direct exposure event.
This rapid progression makes early recognition crucial for any chance of survival.
Signs and Symptoms of the Kerala Brain Eating Amoeba
Because the Kerala brain eating amoeba infection (PAM) mimics common ailments early on, awareness of the symptoms is vital:
- Early symptoms: headache, fever, nausea, vomiting, and stiff neck. These can mirror viral or bacterial meningitis.
- Rapid escalation: confusion, seizures, altered behaviour, hallucinations, loss of consciousness.
- Progression is often measured in days, not weeks. Time from exposure to death is usually less than a week.
- Because the condition is so rare, it is often missed or misdiagnosed, which significantly reduces the chance of survival.
If you or someone you know develops these symptoms after exposure to warm freshwater, immediate medical attention is essential.
Diagnosis and Treatment Challenges
One reason the Kerala brain eating amoeba story is so grim is because of difficulties in diagnosis and limited treatment options:
- Because symptoms resemble common meningitis, doctors may not suspect Naegleria fowleri immediately.
- Confirming diagnosis requires specialized laboratory testing (CSF analysis, PCR) that may not be widely available in remote areas.
- There is no guaranteed treatment. Some drugs, like miltefosine, have been used with limited success. Kerala has improved survival rates through rapid response and newer protocols.
- Globally, the fatality rate is above 95%. In Kerala, thanks to improved systems, mortality has been reduced but remains high.
These limitations make prevention not just better than treatment — it is the only realistic strategy for safety.
Current Numbers and Trends in Kerala
To understand the scale of the Kerala brain eating amoeba issue, here are some recent statistics:
- In 2025, Kerala has reported around 69 confirmed cases and 19 deaths.
- Some reports cite about 80 cases and 21 deaths in 2025 across the state.
- Earlier years had fewer cases — for example, in 2024 the state recorded 29 cases with a lower death rate thanks to interventions.
- Cases are no longer limited to one district, making containment and tracking more complex.
While the absolute number may be small compared to other diseases, the severity and fatality make each case a major concern.
Preventive Measures: How to Protect Against the Kerala Brain Eating Amoeba
Because treatment options are limited, prevention is the key to confronting the Kerala brain eating amoeba threat. Here are recommended steps:
- Avoid swimming or diving in warm freshwater bodies like ponds, lakes, stagnant rivers, or unchlorinated pools.
- Use well-maintained, chlorinated pools and public bathing spaces.
- During nasal irrigation or ritual practices (jala neti), use only boiled, filtered or distilled water—not untreated well or pond water.
- Keep water bodies around homes (wells, storage tanks) clean, properly chlorinated, and avoid allowing them to stagnate.
- Equip local communities with awareness campaigns, signage around risky water bodies, preventive guidelines. Health authorities in Kerala have launched programmes for water sanitation and monitoring.
- If someone experiences early symptoms after freshwater exposure, seek immediate medical evaluation rather than waiting. Time is critical.
These steps may seem simple, but they are powerful in reducing exposure risk.
What Authorities in Kerala Are Doing
In response to the Kerala brain eating amoeba crisis, state and central authorities have taken several actions:
- The Kerala health department launched the “Water is Life” campaign focused on chlorination of wells, tanks and public bathing sites in affected districts.
- Increased surveillance and laboratory testing have been ramped up, with referral networks to major labs for diagnosis of PAM.
- Public advisories have been issued to avoid exposure, use nose-clips, ensure safe water use, and monitor symptoms.
- District-level monitoring of freshwater bodies, improved sanitation, faster response protocols for suspected cases have all been emphasised.
While the threat remains serious, this proactive approach has helped reduce mortality relative to historical norms.
The Broader Implications of the Kerala Brain Eating Amoeba
Though focused on Kerala, the story of the Kerala brain eating amoeba has wider relevance:
- It reminds us that climate, water sanitation and human behaviour interact in complex ways. Warm, stagnant water and inadequate treatment are risk factors worldwide.
- The condition shows how rare diseases can become significant public health issues when environmental and infrastructural vulnerabilities align.
- It highlights the importance of early detection, surveillance, quick outbreak response, public-health education and infrastructure investment.
- For travellers, water-sports enthusiasts, communities relying on natural water sources, this case urges caution and reinforces that vigilance doesn’t require alarm, but informed action.
In short, the lessons from Kerala extend beyond regional borders.
Can the Outbreak Be Controlled?
Yes — with sustained effort, the Kerala brain eating amoeba threat can be reduced significantly.
Control strategies include:
- Ensuring all communal and private wells, tanks, storage systems are properly chlorinated and maintained.
- Establishing clearer guidelines for freshwater recreational use and nasal irrigation practices.
- Strengthening healthcare systems so that suspected cases receive rapid diagnostics and referral.
- Encouraging community education — teaching people why this infection happens and how to avoid it.
- Monitoring environmental changes such as temperature fluctuations and water-body dynamics to anticipate future risk zones.
Given these, while the amoeba may never be fully eliminated (because it’s naturally occurring), human exposure and impact can be drastically minimized.
Conclusion
The term Kerala brain eating amoeba may sound sensational, but behind it lies a sobering reality: a rare, fast-moving infection with grave consequences. However, it is not a hopeless story. With improved awareness, sound infrastructure, careful water use and swift medical response, the dangers can be significantly mitigated.
If you live in Kerala, plan to travel there, or simply love freshwater adventures — remember: the threat is rare, but the precautions matter. By respecting nature, maintaining water safety, and acting quickly on symptoms, we can turn what sounds like a horror-story into a cautionary tale with a positive outcome.
FAQs
What exactly causes the Kerala brain eating amoeba?
It is caused by Naegleria fowleri, an amoeba found in warm freshwater, which enters through the nose and infects the brain.
Can swimming in the sea cause this infection?
No. The amoeba thrives in warm freshwater or poorly treated water, not in seawater which is salty and unsuitable.
Is human-to-human transmission possible?
No. The infection occurs through water entering the nose, not via person-to-person contact.
What are the key symptoms to watch for?
Early: headache, fever, nausea, stiff neck. Later: confusion, seizures, coma. Symptoms escalate rapidly.
How can one protect against the Kerala brain eating amoeba?
Avoid warm stagnant freshwater, use chlorinated pools, ensure safe nasal-irrigation water, maintain household water systems, and monitor early symptoms.
Is the infection always fatal?
Historically, the fatality rate is extremely high (above 95%). But in Kerala improved protocols have helped reduce mortality somewhat.